It is natural to worry about the side effects that may arise when receiving medical radiation as treatment.
The following information outlines some possible tests and treatment options that you may recieve for your diagnosis. Keep in mind that these tests and treatments discussed include ionizing radiation and only represent a portion of tests and treatments that you may recieve.
Included are the effects of these types of radiation and the dose you are exposed to.
Radiation Therapy
If you’ve been diagnosed with SCLC, one of your possible treatment options is radiation therapy. You may or may not be eligible for radiation therapy as the treatment for each individual varies. However, if you are interested in radiation therapy and how it affects you as a patient, this section explains the basics.
What is External Beam Radiation Therapy?
See the following video for what to expect from radiation therapy treatment:
- Radiation therapy utilizes ionizing radiation to kill as many tumour cells as possible and eradicate cancer.
- Uses higher energy photons than in diagnostic x-ray: energy ranges from approx. 4-20 MeV.
- Exposed to a much higher dose of radiation than diagnostic x-ray: prescribed dose depends on treatment site and tumour size.
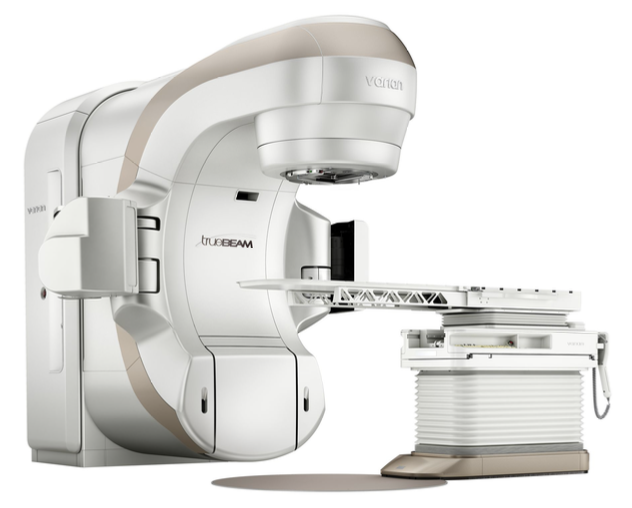
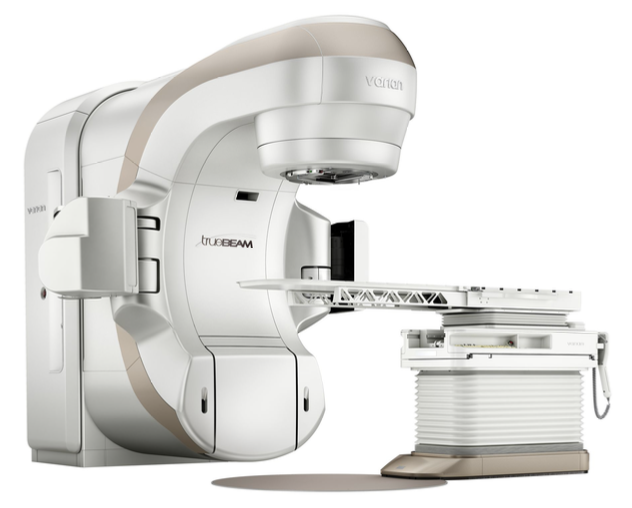
- Linear accelerators (LINACs) are designed to accelerate electrons to high speeds and produce higher energy photons designed for treatment purposes.
- This is what a typical LINAC looks like:
 Precise techniques are used during treatment planning and setup to ensure minimal dose is received by healthy tissue and large dose is received by cancerous cells.
CT simulation is used to determine the position you will be in for all of your treatments and take 3D images of the target anatomy for reference during planning and treatment to ensure accuracy.
Precise techniques are used during treatment planning and setup to ensure minimal dose is received by healthy tissue and large dose is received by cancerous cells.
CT simulation is used to determine the position you will be in for all of your treatments and take 3D images of the target anatomy for reference during planning and treatment to ensure accuracy.
What is Fractionation?
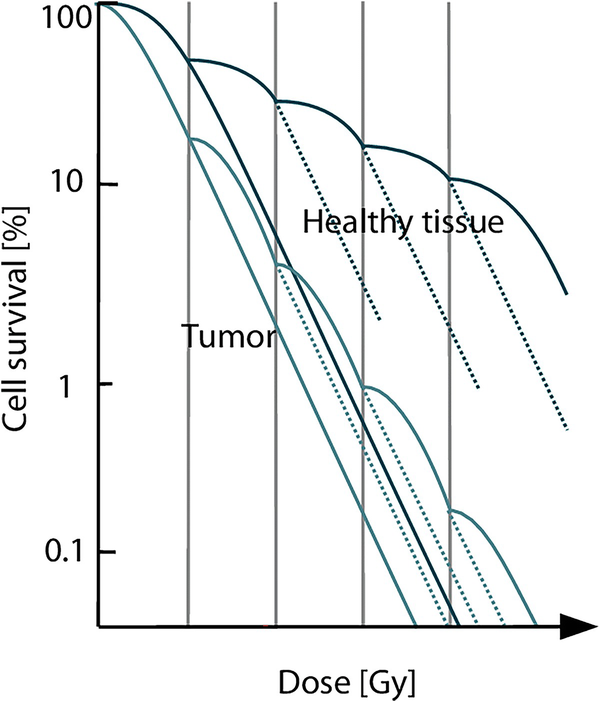
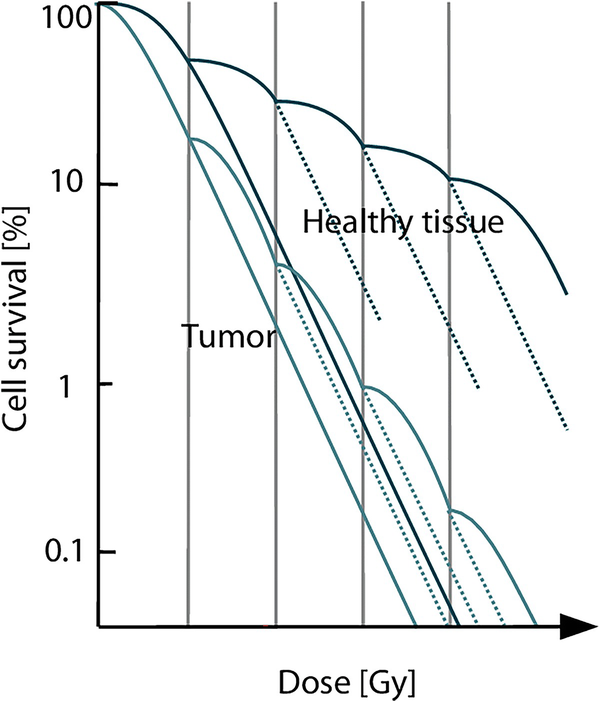
- A large dose is split up into multiple smaller doses over a designated period of time.
- Example: total prescribed dose of 45 Gy, delivered over 30 fractions (split up into 30 smaller doses); therefore each fraction is 1.5 Gy.
- Allows for repair of healthy tissue before the next dose is delivered.
- How is more repair allowed with a smaller dose?
- Theory is that a smaller dose results in less breaks of the DNA per unit volume.
- Less breaks = less surface area for incorrect joining (smaller amount of dangerous aberrations).
- More correct rejoining of chromosomes is likely, due to the small number of broken chromosomes.
What is IMRT?
- Intensity Modulated Radiation Therapy (IMRT) utilizes beams varying in intensity to provide the tumour with the most accurate dose.
- The radiation therapy linear accelerator continuously rotates around the table (and you) while beam-shaping devices (called multi-leaf collimators) shape the beam to the target (tumour).
- This is what a typical IMRT setup looks like:

Image Credit: Cancer Research UK
Doses Used for IMRT
- Current standard doses from Daly et al. (2021):
- 45 Gy, delivered over 30 fractions, and given twice daily (each fraction = 1.5 Gy), given 3 Gy in one day.
- 60-70 Gy, delivered over 30-35 fractions, given once daily (each fraction = 2.0 Gy), given 2 Gy in one day.
How is my Body Affected by IMRT?
- Side effects depend on MANY factors, some effects may be reduced if you are receiving chemotherapy or have a smaller treatment field (tumour).
- Skin (signs and symptoms begin appearing 2-3 weeks after the start treatment): erythema (redness), dryness, pigmentation changes, fibrosis (late stages), temporary hair loss (where radiation enters the body).
- Temporary hair loss occurs approximately 3 weeks after an exposure to 3-6 Gy, with regrowth beginning approximately 2 months after radiation treatment is completed (Bushberg et al., 2020).
- Lymphocytes (WBCs): temporary decreased count = decreased immune system (more prone to acquiring infections, viruses, etc.).
- GI System: oesophagitis (inflammation of the esophagus mucosal wall) = sore throat, difficulty swallowing.
- Lung Structures: pneumonitis (inflammation of lung tissue) and a dry non-productive cough (resulting from irritation of trachea and bronchus) are both considered chronic or late effects (Washington et al., 2021).
- Heart Problems - swelling of tissue surrounding the heart: pain, abnormal heart rhythm (late effects).
What is PCI?
- Prophylactic cranial irradiation (PCI) may be used for patients with higher stages of SCLC to reduce the risk of brain metastases.
- You may not be eligible for PCI if: you are older than 60, you have neurocognitive impairment or have a poor general performance status.
- It is important to note that approximately 60% of patients with tumours located in the thorax develop metastases in the brain (Suwinski, 2021).
- Your oncologist will order MRI or PET images of your brain to look for any signs of cancer that is present but difficult to detect via imaging.
- If your oncologist decides that you do not need PCI, you will still need multiple follow-up MRIs to ensure no spread has occurred.
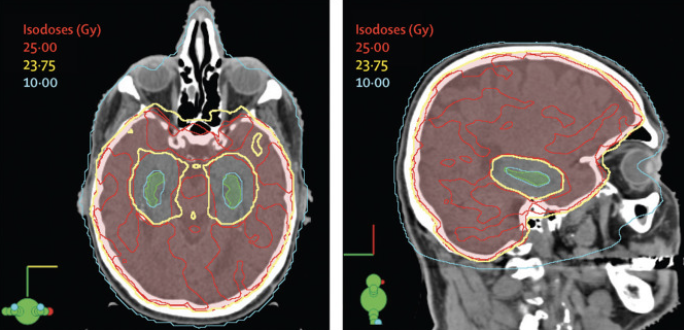
- This is what a typical PCI setup looks like:
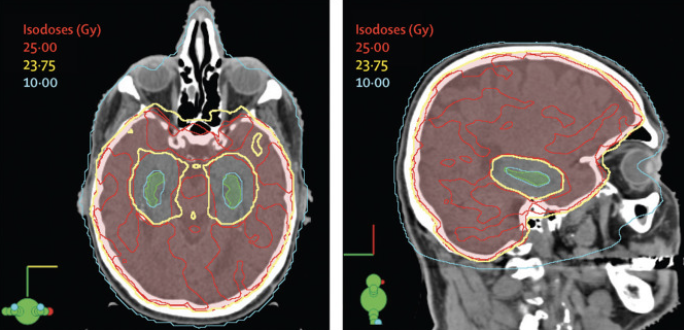
Image Credit: The Lancet
Doses Used for PCI
- Current standard dose from Suwinski (2021):
- 25 Gy delivered over 10 fractions, given once daily (each fraction = 2.5 Gy).
How is my Body Affected by PCI?
- Decline in memory may be observed at approximately 1 year post-irradiation (Suwinski, 2021).
- Fatigue, appetite loss, nausea, and leg weakness for up to 3 months due to temporary swelling of brain tissue as an acute response to radiation (Edelman, 2020).
- However, neuropsychological impairment could be connected to the cancer itself or to treatment given before PCI (Péchoux et al., 2016).
- Improvements have been made to significantly reduce dose to critical structures such as the hippocampus.
- Whole-brain irradiation for brain metastases while sparing the hippocampus was associated with the preservation of memory and quality of life and these practices may be introduced into PCI to lessen the side effects and improve quality of life (Péchoux et al., 2016).
- Hippocampus plays an important part in brain injury repair, so sparing this portion of the brain from radiation is important.
Bottom Line
When considering treatment for cancer, it is always important to weigh the costs and benefits of a specific procedure. Radiation therapy for the treatment of lung cancer has been used for several decades and proven to be a reliable treatment option. Although there are side effects involved with receiving radiation, the effectiveness of radiation at eradicating cancer outweighs the cost of these side effects. Your healthcare team of radiation therapists and oncologists will provide you with the most superior care and assist you with side effect management and treatment for any radiation associated side effects.
References
- Bushberg, J. T., Seibert, J. A., Leidholdt, E. M., & Boone, J. M. (2020). The essential physics of medical imaging (4th ed.). Wolters Kluwer.
- Daly, M. E., Ismaila, N., Decker, R. H., Higgins, K., Owen, D., Saxena, A., Franklin, G. E., Donaldson, D., & Schneider, B. J. (2021). Radiation therapy for small-cell lung cancer: ASCO guideline endorsement of an Astro guideline. Journal of Clinical Oncology, 39(8), 931–939. https://doi.org/10.1200/jco.20.03364
- Edelman, M. J. (2020). Prophylactic cranial irradiation for small-cell lung cancer: Time for a reassessment. American Society of Clinical Oncology Educational Book, (40), 24–28. https://doi.org/10.1200/edbk_281041
- Péchoux, C. L., Sun, A., Slotman, B. J., De Ruysscher, D., Belderbos, J., & Gore, E. M. (2016). Prophylactic cranial irradiation for patients with lung cancer. The Lancet Oncology, 17(7). https://doi.org/10.1016/s1470-2045(16)30065-1
- Small cell lung cancer (SCLC) - external beam radiation therapy (EBRT). eviQ. (2023). https://www.eviq.org.au/radiation-oncology/respiratory/4292-respiratory-small-cell-lung-cancer-thoracic-e/patient-information#side-effects
- Suwinski, R. (2021). Prophylactic cranial irradiation in SCLC. Translational Lung Cancer Research, 10(4), 2071–2078. https://doi.org/10.21037/tlcr-2020-rtm-05
- Washington, C. M., Leaver, D. T., & Trad, M. (2021). Washington and Leaver’s principles and practice of radiation therapy. Elsevier.
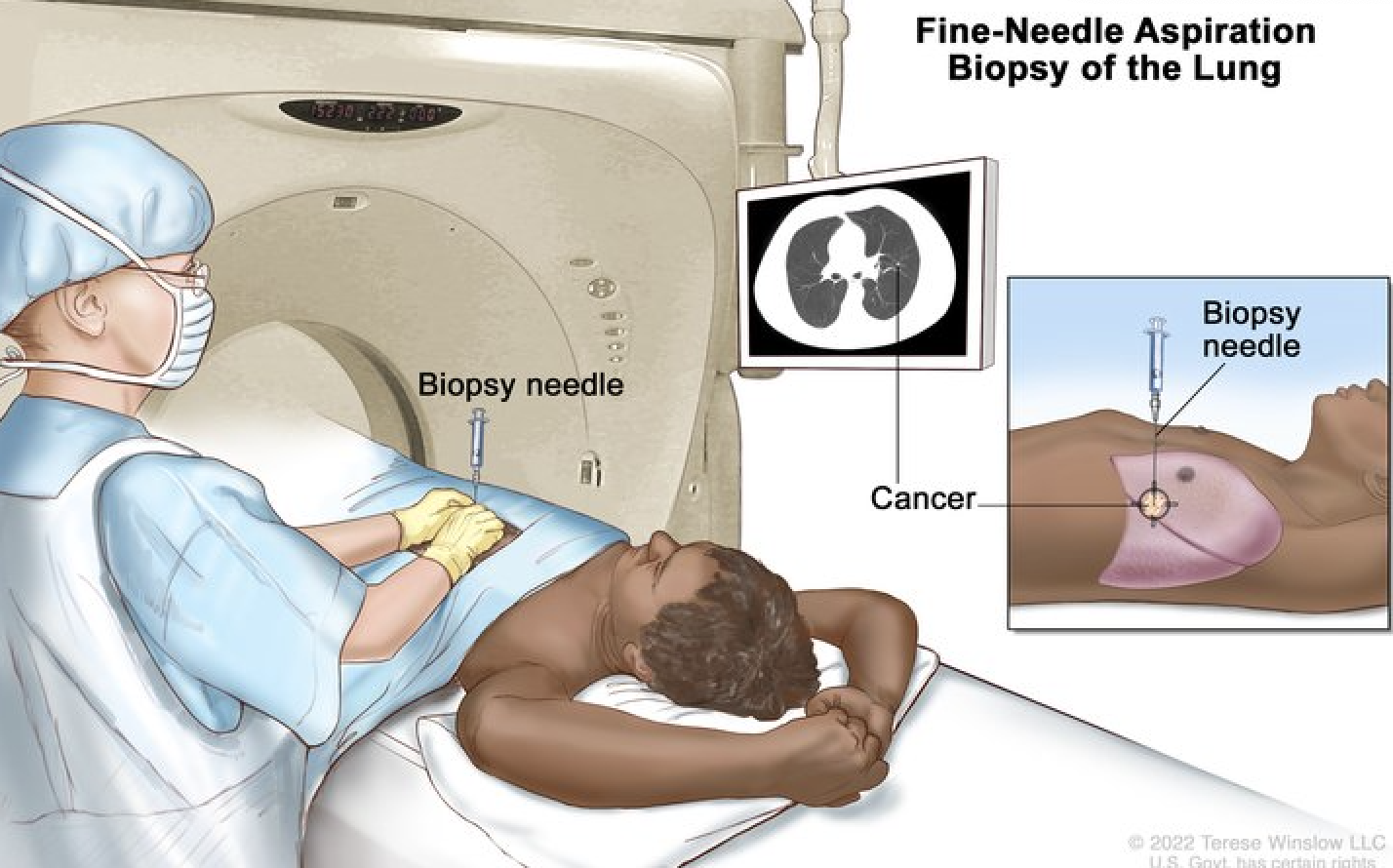
Radiation Exposure from CT-Guided Fine Needle Aspiration (FNA) in SCLC
If you've been diagnosed with small cell lung cancer (SCLC) and your doctor recommends a CT-guided fine needle aspiration (FNA) to check a suspicious lung lesion, you might wonder about the radiation exposure. Here’s a simple breakdown of what you need to know:
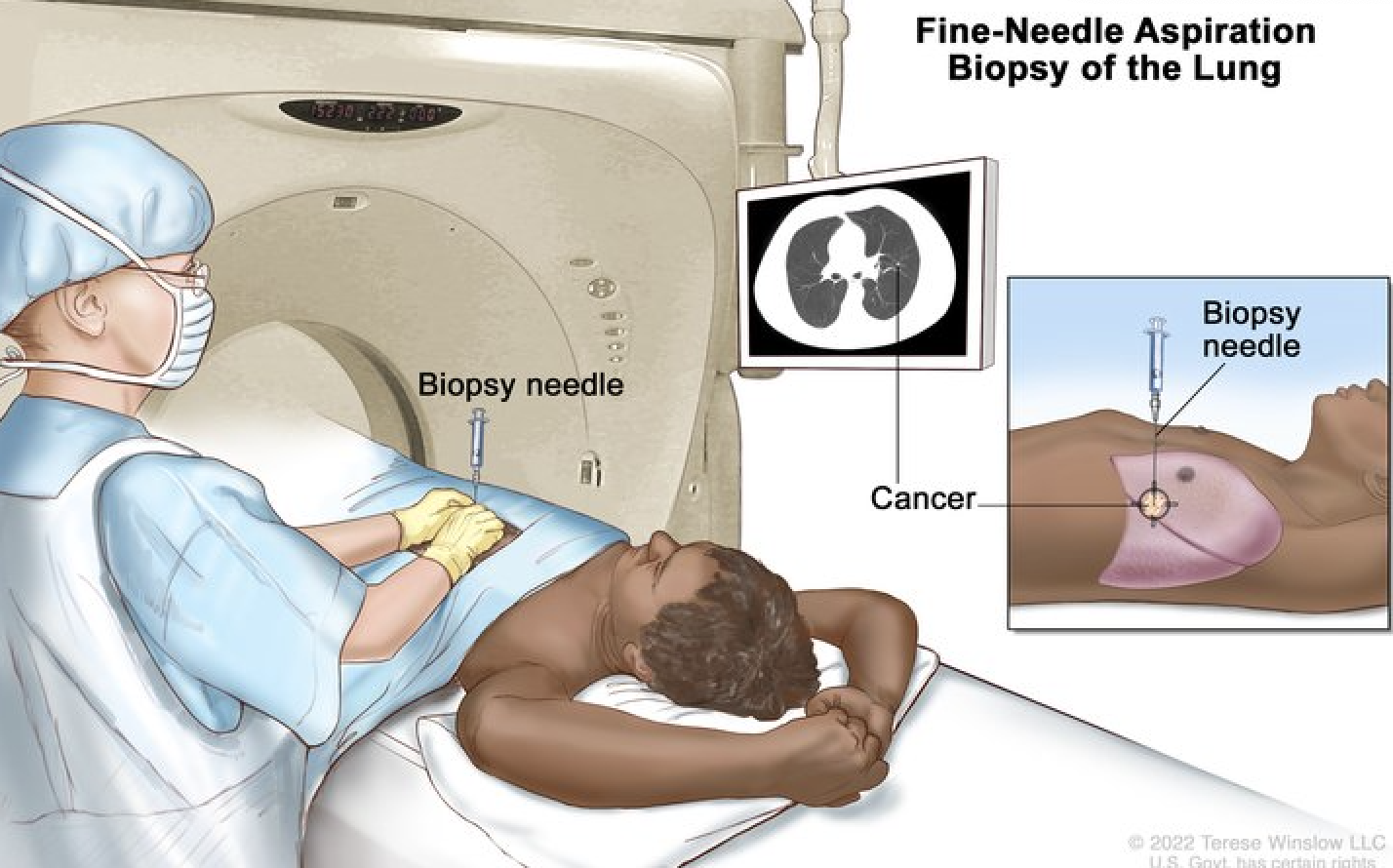
- What is CT-Guided FNA?
CT-guided FNA is a minimally invasive biopsy that uses a thin needle to take a small sample from your lung. A CT scan (computed tomography) helps guide the needle precisely to the right spot (National Cancer Institute [NCI], 2023).
- How Much Radiation is Involved?
A CT-guided FNA usually exposes you to 1–7 mSv, which is:
- Lower than a full chest CT scan (5–7 mSv)
- Higher than a chest X-ray (0.1–0.2 mSv) (Bushberg et al., 2020)
If you need more than one biopsy, your exposure adds up over time, but doctors use low-dose techniques to keep it as low as possible.
- Is Radiation Harmful?
The radiation from one or a few procedures is very unlikely to cause harm. Long-term risks are small, but repeated exposure over time may slightly increase the chance of cancer in the future (NCI, 2023). The benefit of diagnosing and treating your cancer outweighs this small risk.
- Which Body Parts Are Affected?
Lungs receive most of the radiation, while the breast and thyroid receive minimal exposure (Bushberg et al., 2020).
- Radiation Exposure to Medical Staff:
Medical teams use protective shields and distance techniques to minimize their own exposure (NCI, 2023).
Bottom Line: CT-guided FNA is an important diagnostic tool for SCLC. Radiation risk is very low compared to the benefits of early and accurate diagnosis. If concerned, discuss dose-reduction options with your doctor.
References
- Bushberg, J. T., Seibert, J. A., Leidholdt, E. M., & Boone, J. M. (2020). The essential physics of medical imaging (4th ed.). Wolters Kluwer.
- National Cancer Institute (NCI). (2023). Computed tomography (CT) scans and cancer risk. Retrieved from https://www.cancer.gov/about-cancer/diagnosis-staging/ct-scans-fact-sheet
Radiography
Who is most at risk of developing SCLC?
- SCLC mostly occurs in individuals in their early to late 60s and is linked to cigarette smoking, with the majority of patients having a history of tobacco use (Dumoulin et al., 2023; Wang et al., 2023).
- SCLC represents about 14% of all lung cancer cases.
- Individuals of African ancestry are at lower risk of developing SCLC compared to those of European ancestry.
Why is a chest X-ray the most common procedure for diagnosing or suspecting SCLC?
A patient with or suspected of having SCLC would normally undergo a chest X-ray (CXR) before other imaging modalities are considered.
The reason CXR is commonly used is due to:
- Their low cost
- Easy accessibility
- Minimal radiation exposure, with a single CXR involving a dose of approximately 0.02 mSv (Bradley et al., 2019; Public Health England, 2008).
- While the radiation dose from a single CXR is minimal, repeated X-rays over time can add up.
- This is especially important for SCLC patients, who often require frequent imaging, such as PET (discussed later on), to track the progression of the disease and the effectiveness of treatment.
- Thus, the combined exposure over time can increase the risk of long-term side effects, such as a slightly higher chance of developing other cancers later in life.
- However, this risk is generally small compared to the immediate benefits of accurately diagnosing and treating SCLC.

Figure 1. A patient prepared for a chest X-ray (Laguna Beach Urgent Care, 2025).
What are some benefits and drawbacks of using chest X-rays for diagnosing SCLC?
- Any X-ray view required in radiography is painless, quick, and non-invasive, typically taking only a few minutes to complete.
- There are no immediate side effects from the radiation used in a single CXR.
- An advantage of using CXR to diagnose SCLC is that a resulting radiograph can reveal large masses, fluid buildup, or other abnormalities in the lungs that may indicate SCLC.
- However, some studies have indicated that CXR is less effective at detecting small tumours or early-stage SCLC (Bradley et al., 2019).
- This can lead to delayed diagnosis, which is concerning given the aggressive nature of SCLC.
- CXRs provide limited information about whether the cancer has spread (metastasized) to other parts of the body.
- Advanced imaging like CT or PET scans are required for staging.
- Studies demonstrated that approximately 90% of missed lung cancer cases occur on CXR.
- This is often attributed to factors such as misinterpretation of pathological findings as normal, the size and location of tumours, and variations in the skill level of those interpreting the radiograph (Del Ciello et al., 2017).
- CXRs sometimes produce false positives, such as mistaking benign conditions for cancer, or false negatives, such as failing to detect small tumours. This can lead to unnecessary follow-up tests or overlooked diagnoses.
References
- Del Ciello, A., Franchi, P., Contegiacomo, A., Cicchetti, G., Bonomo, L., & Larici, A. R. (2017). Missed lung cancer: When, where, and why? Diagnostic and Interventional Radiology (Ankara, Turkey), 23(2), 118–126. https://doi.org/10.5152/dir.2016.16187
- Bradley, S. H., Abraham, S., Callister, M. E., Grice, A., Hamilton, W. T., Lopez, R. R., Shinkins, B., & Neal, R. D. (2019). Sensitivity of chest X-ray for detecting lung cancer in people presenting with symptoms: A systematic review. British Journal of General Practice, 69(689), e827–e835. https://doi.org/10.3399/bjgp19X706853
- Dumoulin, D. W., Aarts, M. J., De Ruysscher, D., Aerts, J. G. J. V., & Dingemans, A.-M. C. (2023). Trends in the epidemiology of small-cell lung cancer: A Dutch nationwide population-based study over 1989–2020. European Journal of Cancer, 191, 112985. https://doi.org/10.1016/j.ejca.2023.112985
- Laguna Beach Urgent Care. (2025). Chest x-rays uncovered: What they show, how long they take, and more. [Photograph]. https://lagunabeachuc.com/inside-chest-x-rays/
- Public Health England. (2008, September 4). Patient dose information: guidance. GOV.UK. https://www.gov.uk/government/publications/medical-radiation-patient-doses/patient-dose-information-guidance
- Wang, Q., Gümüş, Z. H., Colarossi, C., Memeo, L., Wang, X., Kong, C. Y., & Boffetta, P. (2023). SCLC: Epidemiology, risk factors, genetic susceptibility, molecular pathology, screening, and early detection. Journal of Thoracic Oncology, 18(1), 31–46. https://doi.org/10.1016/j.jtho.2022.10.002
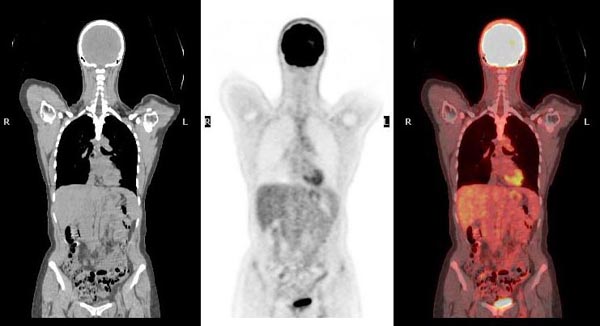
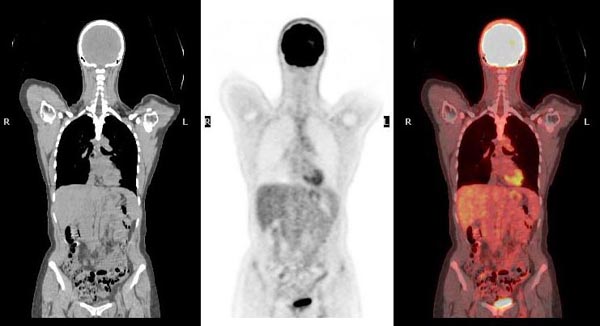
Positron Emission Tomography (PET)
Positron emission tomography (PET) also serves as another imaging modality that can help detect the presence of SCLC tumour cells or any possible spread to other parts of the body of the patient (Treadwell et al., 2016).
Is PET safe for my body?
- PET uses ionizing radiation and radiotracers to localize positron-emitting radioisotopes in the body, which are key for showing the SCLC tumour on a PET scan image.
- An example of many of the radiotracers used would be Fluorine-18 Fluorodeoxyglucose (18F-FDG).
- Radiotracers emit gamma rays, which are a form of ionizing radiation (World Nuclear Association, 2025).
- 18F-FDG has a short half-life of less than 2 hours. This means that it does not remain in the body for too long and can be evacuated through urine and stool, which contributes to the safety of undergoing PET scans.
- Therefore, there is no significant effect from radiation from a single PET scan.
What can PET bring to SCLC patients?
An advantage of using PET with the 18F-FDG radiotracer is the ability to distinguish tumours such as SCLC from nodules or masses, which are often mistaken for tumours or other pathologies and cannot be detected with other imaging modalities.
- However, a disadvantage of PET is that the resulting images would not be able to show the necessary anatomical details that would help the doctor diagnose a patient.
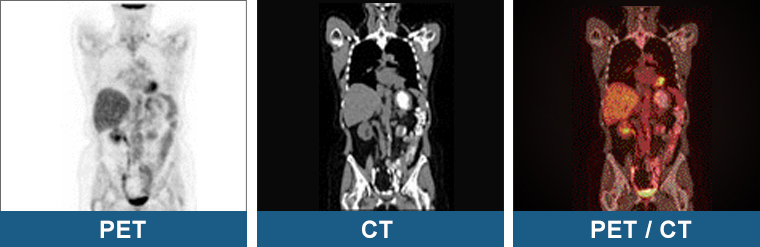
How can PET be combined with other imaging modalities?
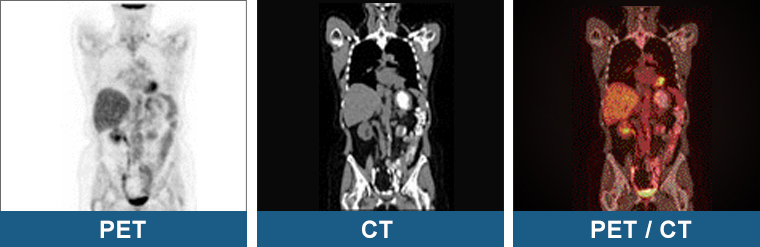
- Usually, a PET scan can be combined with other imaging modalities and performed at the same time, such as CT, creating what is called a PET-CT scan (Treadwell et al., 2016).
- A PET-CT scan would compensate with the necessary anatomical details that would not be demonstrated if PET alone were used.
Why is SCLC often found after it has spread and what role PET scans play to help spot any pathologies?
- Research has shown that SCLC is a very aggressive type of cancer, which means it tends to spread to other parts of the body quite quickly, even in early stages (Decoster et al., 2008).
- By the time SCLC is diagnosed, in about 7 out of 10 people, the cancer has already spread to multiple sites, making it harder to treat.
- Due to the metastatic nature of SCLC as a cancer, SCLC patients may have an elevated 18F-FDG activity on PET scans in a certain area.
- This means that those areas are using a lot of glucose (sugar). This is called being “FDG-avid.”
- This is not something to worry about as being FDG-avid is only a term to indicate that cancer is present, but sometimes it could just be inflammation, an infection, or other pathologies within the patient (Hofman & Hicks, 2016).
- For example, in the same study by Hofman & Hicks (2016), an early-stage (T1N0) patient had an 18F-FDG lesion in their lower right abdomen.
- This simply means that the PET scan picked up a spot with increased activity, which might need further investigation, but is not necessarily alarming on its own.
- As a result, cancer cells will show up as bright spots on PET scan images.
Common Concerns that You May Have:
- It is very common for patients to be afraid of getting a PET scan immediately after learning that it involves ionizing radiation.
- The amount of radiation a patient can be exposed to during a PET scan is in the range of 8 mSv (millisieverts) for adults, which is approximately the same as the radiation expected to be received naturally from the sun (Kapoor & Kasi, 2022).
- Pregnant women should avoid these scans unless absolutely necessary because the radiation could harm the fetus or embryo, especially if during the pre-implantation stage of pregnancy.
- Breastfeeding mothers should stay away from babies and pregnant individuals for about 12 hours after undergoing a PET scan.
- Lactating women are required to throw out breast milk for the first 12 hours. After 24 hours, it is generally safe to breastfeed again.
- Risks of PET:
- The risk of PET is considered low or modest compared to the benefits it provides in the diagnosis and treatment of pathologies.
- Scientists have also shown that patients with SCLC (specifically limited stage) who had undergone a PET scan had shown better disease control and longer survival compared to non-PET staged SCLC patients (Xanthopoulos et al., 2013).
- Your doctor would normally weigh this small risk against the need for accurate medical information to guide treatment.
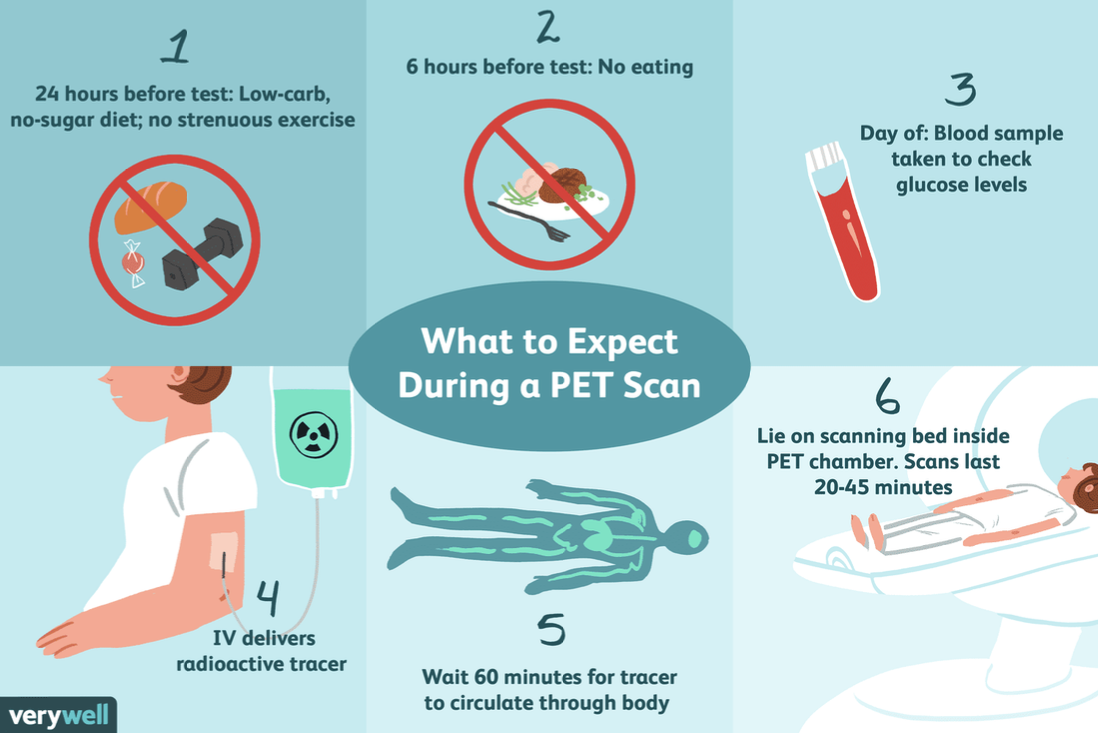
How to Prepare for a PET Scan and What to Expect?
- Two days before your PET scan appointment: No intense exercises or deep-tissue massages (Cedars-Sinai, 2025).
- One day before: No sugary or starchy foods like bread, pasta, or rice.
- On the day: Don't eat or drink for 6 hours before, except plain water or medications.
- Bring your doctor’s requisition (if they give you one).
- Leave jewelry, metals, hairclips, dental appliances, and important stuff at home. You can bring your glasses (if you wear one) but you will have to remove them.
- A PET procedure starts with the technologist introducing a positron-emitting radiotracer in the vein of the patient, which accumulates in the target tissue (Kapoor & Kasi, 2022). Then, the PET scanner will rotate around the patient to produce images of areas inside the body where the radiotracer has taken up.
- The resulting PET image produced would help the doctor to detect, diagnose, or stage SCLC, offering appropriate treatment.
- You might feel temporary minor discomfort at the site of radiotracer injection or a warm sensation after it is injected (Cleveland Clinic, 2022). Allergic reactions are rare but can occur.
- A PET scan usually takes approximately 1 hour to complete (Cedars-Sinai, 2025).
- Take a look at the following video to learn more about what to expect during your PET scan: https://www.youtube.com/watch?v=d9iOxMFmPlA
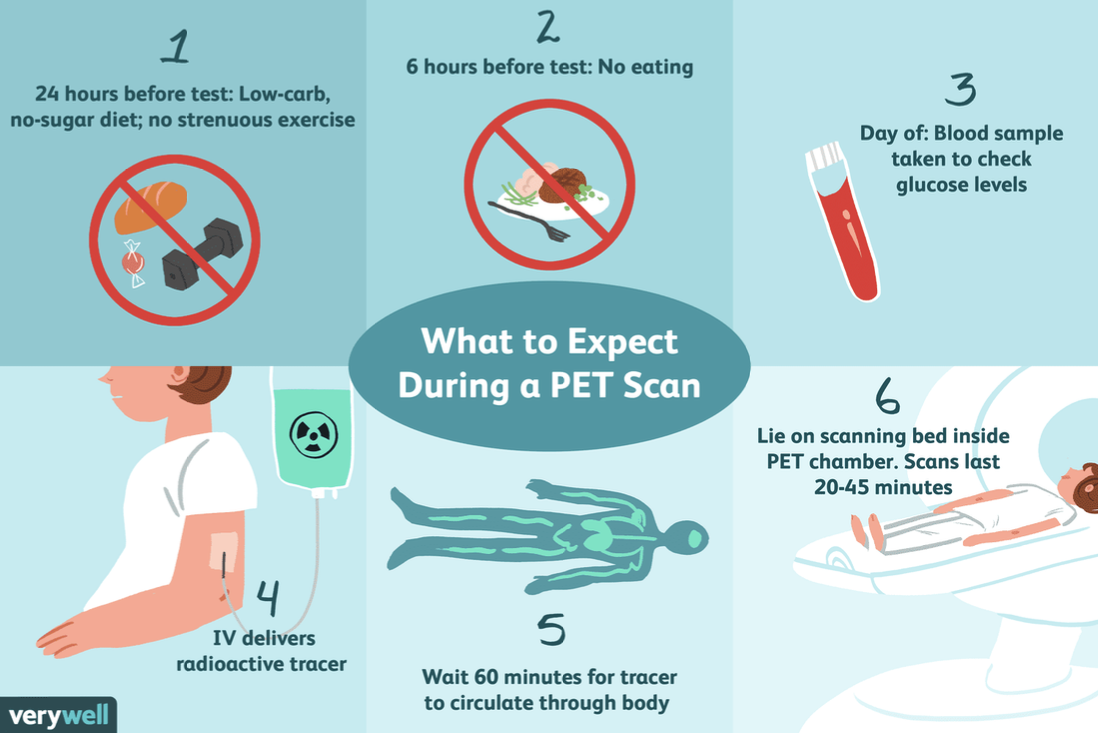
Figure 2. PET scan procedure and considerations (Raymaakers, 2024).
References
- Cedars-Sinai. (2025). FDG-PET scan. Cedars-Sinai. https://www.cedars-sinai.org/programs/imaging-center/exams/pet-ct-scans/fdg-pet-scan.html
- Cleveland Clinic. (2022, October 19). PET scan. https://my.clevelandclinic.org/health/diagnostics/10123-pet-scan
- Decoster, L., Stroobants, S., Verbeken, E., Nackaerts, K., & Vansteenkiste, J. (2008). An unexpected abdominal 18F-Fluorodeoxyglucose (FDG) uptake on positron emission tomography (PET) in a patient with limited stage small cell lung cancer. Journal of Thoracic Oncology, 3(2), 174–176. https://doi.org/10.1097/JTO.0B013E318162336B
- Hofman, M. S., & Hicks, R. J. (2016). How we read oncologic FDG PET/CT. Cancer Imaging, 16(1), 35. https://doi.org/10.1186/s40644-016-0091-3
- Kapoor, M., & Kasi, A. (2022, October 3). PET scanning. In StatPearls. Treasure Island, FL: StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK559089/
- Treadwell, J. R., Mitchell, M. D., Tsou, A., et al. (2016, April). Imaging for the pretreatment staging of small cell lung cancer. Comparative Effectiveness Reviews, No. 174. Rockville, MD: Agency for Healthcare Research and Quality (US). Retrieved March 11, 2025 from https://www.ncbi.nlm.nih.gov/books/NBK362055/
- Raymaakers, K. (2024, October 13). PET scan: Purpose, procedure, and side effects. Verywell Health. https://www.verywellhealth.com/what-to-expect-during-a-petct-scan-2252467
- UW Medicine. (2010, December 20). PET (positron emission tomography) scan: What to expect [Video]. YouTube. https://www.youtube.com/watch?v=d9iOxMFmPlA
- World Nuclear Association. (2025). Radioisotopes in medicine. https://world-nuclear.org/information-library/non-power-nuclear-applications/radioisotopes-research/radioisotopes-in-medicine
- Xanthopoulos, E. P., Corradetti, M. N., Mitra, N., Fernandes, A. T., Kim, M., Grover, S., Christodouleas, J. P., Evans, T. L., Stevenson, J. P., Langer, C. J., Lee, T. T., Pryma, D. A., Lin, L. L., Simone, C. B., Apisarnthanarax, S., & Rengan, R. (2013). Impact of PET staging in limited-stage small-cell lung cancer. Journal of Thoracic Oncology, 8(7), 899–905. https://doi.org/10.1097/JTO.0B013E31828E8996