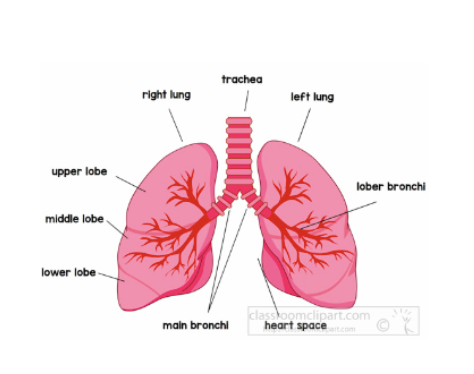
The cumulative radiation dose from the diagnosis and treatment of small cell lung cancer
is influenced by various patient-specific factors, including age, body habitus, lifestyle
choices, tumor location, pregnancy status, and genetic predispositions. As radiation
exposure plays a crucial role in both diagnosing and treating this aggressive cancer,
personalized treatment planning and advanced radiation delivery techniques are essential
for optimizing therapeutic outcomes while minimizing the risks of adverse effects.
Ongoing research into radiotherapy techniques and protective measures is vital to
improving the safety and efficacy of SCLC treatments, ensuring better outcomes for all
patients, regardless of their individual risk factors.