Diagnosis: CT
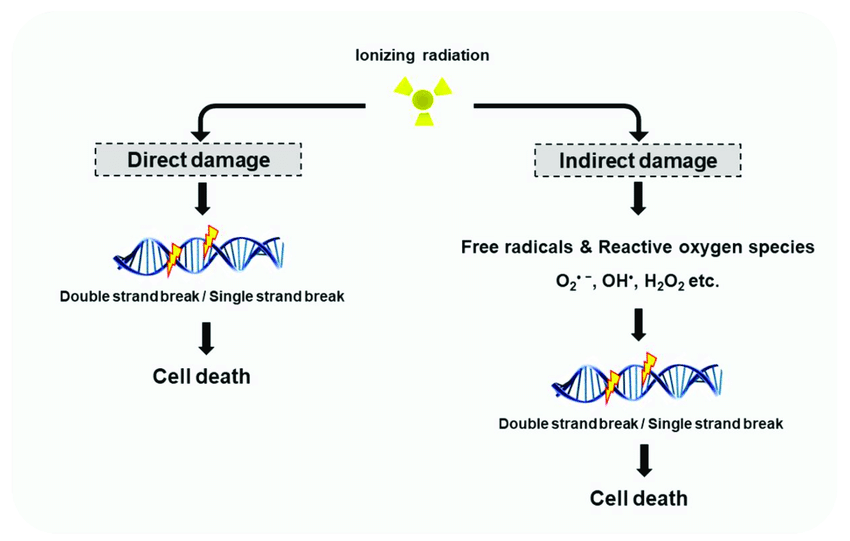
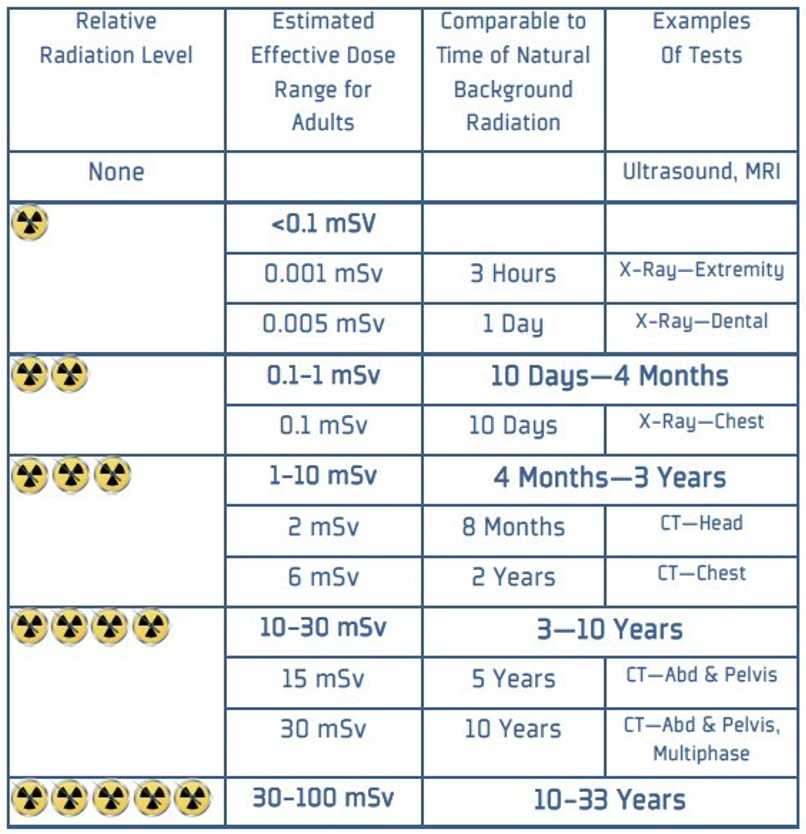
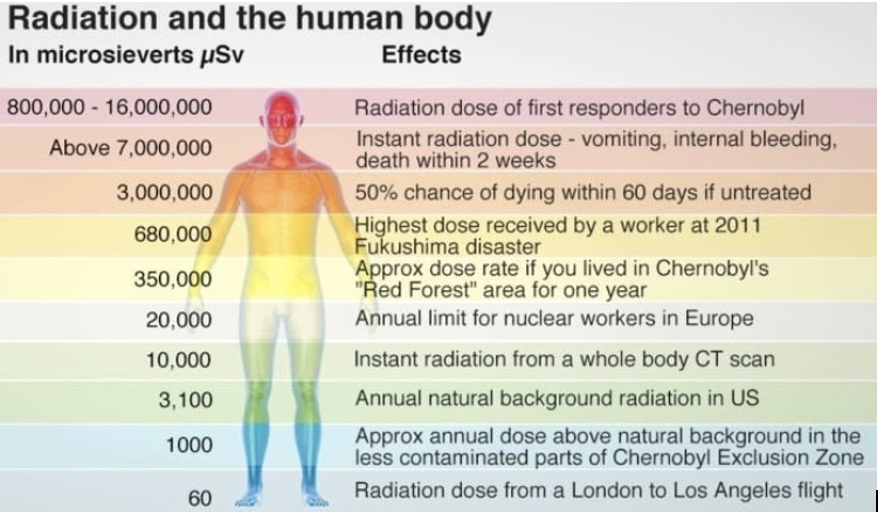
CT uses x-rays, which is a form of ionizing radiation. Ionizing radiation is defined as radiation that has undergone ionization (Hall & Giaccia, 2019).
- Ionization occurs when radiation has enough energy to eject an orbital electron from a molecule or atom.
- Large amounts of energy being released locally is a key characteristic of ionizing radiation (Hall & Giaccia, 2019).